Posted on February 26, 2016
by Cheri Harkleroad
This guide offers all the essential information about naloxone – the lifesaving antidote for opioid overdose.
The information here is NOT a substitute for medical advice – it is intended to serve as a general guide to increase overall awareness of naloxone. ALWAYS seek information from your doctor or pharmacist.
According to the CDC there were 47,055 drug overdose deaths in the United States in 2014, 28,647 of these deaths (61%) involved some type of opioid, including heroin.” – Center for Disease Control
Knowing how to use naloxone to reverse an overdose could mean the difference between life and death. By now most people have heard about naloxone, even if they’re not quite sure what it is. Naloxone (Narcan, Evzio) has been a hot topic in the news and in public health policy as a proactive measure against the dramatic increase in American overdose deaths. This is the essential guide for everything you need to know about naloxone.
What is naloxone?

Naloxone is a medication that serves as an antidote to opioid overdose. Naloxone works by reversing respiratory depression caused by opioid (natural, semi-synthetic and fully synthetic) drugs, including:
- Opium
- Morphine
- Codeine (Tylenol 3, Tylenol w/ Codeine)
- Heroin
- Hydromorphone (Dilaudid)
- Hydrocodone (Vicodin)
- Oxycodone (Oxycontin, Percocet, Percodan, Tylox)
- Buprenorphine
- Fentanyl
- Methadone
Naloxone does NOT work in cases of overdose from substances such as:
What is the difference between an opiate and an opioid?
Opioid is the broader class and includes opiates. For simplicity, we use one term only, opioid.
Is Narcan the same as naloxone?
Naloxone is the generic name of the medication sold under brand name labels of Narcan and Evzio.
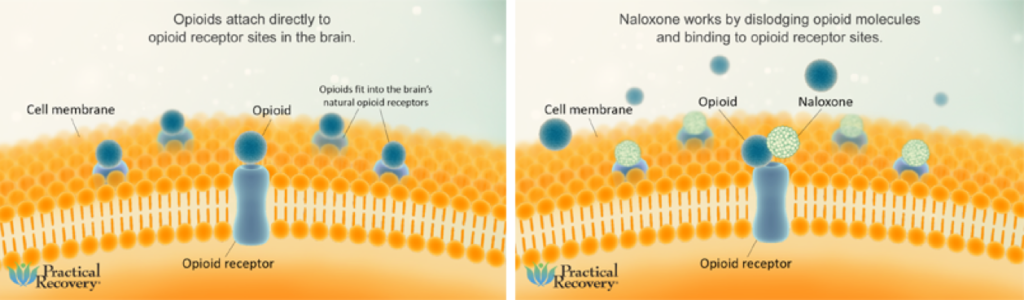
How does naloxone work?
Opioids slow your breathing, potentially ceasing breathing function altogether. Naloxone works by binding to opioid receptors in the brain and inhibiting the uptake of opioid molecules. In doing so, the overdose can be reversed and respiratory function can resume.
Is naloxone effective?
Yes! Naloxone saves lives. There is no denying it.
From 1996 through June 2014, surveyed organizations provided naloxone kits to 152,283 laypersons and received reports of 26,463 overdose reversals. Providing opioid overdose training and naloxone kits to laypersons who might witness an opioid overdose can help reduce opioid overdose mortality.” – Center for Disease Control and Prevention
When to use naloxone:
Use of naloxone is recommended in the event of a suspected opioid overdose. During an opioid overdose, a person may exhibit one or all of these symptoms (key indicators in bold):
- The person may have a purple/black hue on the lips and/or fingernails
- The person does not respond to external stimuli
- Breathing may be slow/shallow/erratic or may have stopped completely
- You may hear the person making strange snoring, choking or gurgling noises (“death rattle”)
- The person may be awake, but is unable to communicate
- The person may be limp; deadweight
- The person may be pale and/or clammy
- A purple hue in the skin of light skin-toned people, and a grayish or ashen appearance in those with darker skin
- Pulse may be slow/weak/erratic or may have stopped completely
- The person may vomit
- Fluids may come from the nose and/or mouth
- The person may become unconscious
If you notice these signs, whether one or several, respond right away.
If the person appears unconscious, shout their name and shake them. Do they respond? If the answer is no, try eliciting a pain response by rubbing your knuckles over their sternum or, if you can’t get to their sternum, rub just above their upper lip area, beneath the nose. The goal here is to see if they react to mild pain. If they do not react immediately, move on as this is likely a life threatening situation and time is of the essence.
Call 911, start rescue breathing if necessary and prepare to administer naloxone.
It is important to note the majority of drug poisoning deaths involve more than one drug; however, naloxone is effective even in these cases so long as one of these drugs is an opioid. Even if none of the drugs is involved is an opioid, naloxone is harmless. Therefore, if you even suspect that one of the drugs involved in the overdose might be an opioid, use naloxone!” – Kenneth Anderson, hamsnetwork.org
Recognize the major signs of overdose
How to use naloxone injection:
- According to Sharon Stancliff, MD of org, whether you call 911 or give naloxone first depends on which is more readily accessible. The point is to intervene as quickly as you can and call for additional help.
- Use a needle to inject 1cc (1mL/100u) of the medication directly into a muscle or under skin (thigh or shoulder are best), administering through victim’s clothing if necessary. Buttocks injections increase the risk of sciatica, especially when given by untrained individuals.
- Continue rescue breathing for a few minutes while the medication takes effect
- Administer a second dose of naloxone if the first one isn’t effective
- Continue rescue breathing (or CPR if trained)
- If breathing is restored, position person’s body in the recovery position
- Stay with the victim until emergency help arrives! Even with successful reversal of overdose symptoms, the person can still revert to an overdose state if the medication wears off before the opioids.
How to use intranasal naloxone:
It is important to know that one dose of nasal naloxone comes as a kit with 3 pieces: an atomizer (tip that is inserted into nostril), applicator (tube with a removable yellow piece at each end) and a glass vial of medication. All three items are included with an intranasal naloxone kit and are necessary for administration.
- Call 911
- Remove yellow ends from applicator
- Remove cap from vial (cap will either be purple or red and should easily pop off)
- Gently Insert open end of vial into open end of applicator and twist until you feel slight resistance
- Attach atomizer to assembled vial and applicator unit
- Insert atomizer into one nostril of overdose victim and spray half dose by pushing vial into applicator
- Insert atomizer into other nostril and spray remaining dose
- If breathing is restored, position the person’s body in the recovery position
Just as with naloxone injection, wait 2 or 3 minutes to see if the medication starts working. If no sign of symptoms reversing, administer a second dose and continue rescue breathing as you wait for help. The opiates that caused the overdose may outlast the naloxone so be sure to watch for signs that the person is returning to a state of overdose.
How to Administer Naloxone in the Event of an Opiate Overdose
How long does naloxone last?
Naloxone lasts 30-90 minutes. It is important to know that the effects of opioids, including respiratory arrest, can last several hours, while naloxone will last anywhere from half an hour to an hour and a half. This means that even if the naloxone is effective in reversing the overdose, it could wear off before the opioids and the individual would again be at risk for overdose. Stay with the person until you are certain the opiates have worn off or until help arrives.
Naloxone side effects:
According to harmreduction.org, naloxone does not have any side effects, even if an individual is not overdosing and/or has no opiates in their system. While the medicine does not have any contraindications, for someone who is opiate-dependent, administration may cause symptoms of withdrawal. Withdrawal symptoms are positively correlated with the amount of naloxone received. That is, the more naloxone administered, the stronger the feelings of withdrawal.
If a person is feeling symptoms of withdrawal after administration of naloxone, the site also suggests letting the person know that the “dopesickness” will only last about half an hour or so. It is important to encourage the person to wait it out, instead of using more drugs to counteract the discomfort, as this can put them at risk for another overdose as soon as the naloxone begins to wear off.
Does naloxone make people violent?
Naloxone itself does not make people violent. If someone exhibits agitation or violence upon arousal from the overdose state, this is likely due to confusion and possible symptoms of withdrawal. In the case of such agitation, talking to the victim is suggested. Explain what happened and let them know that any feelings of withdrawal will wear of as the medication wears off.
Intranasal or intramuscular naloxone – which is better?
Both are excellent, and deciding which one to use is a personal decision. It should be noted, however, that intranasal naloxone eliminates the risk of needle stick to the person administering the drug. This can be especially beneficial when administering the medication to a known intravenous drug user (IVDU). IVDUs belong to a population at high risk for contracting blood-borne pathogens such as Hepatitis C (HCV) and Human Immuno-deficiency Virus (HIV).
Can I get high on naloxone?
You cannot get high on naloxone. If it is used by someone who has no opiates in their system, it would have the same effect as water. The medication has no potential for abuse or dependency.
Is naloxone safe for everyone?
Yes. While the kit to administer naloxone (small parts, fragile glass vial, needle) could potentially cause harm to small children and pets, the medication itself is relatively safe. The medication only inhibits the binding of opiates to receptors in the brain. If there are no opiates present, the medication does not do anything, except in the unlikely event of a severe allergic reaction.
It is listed as a Schedule C medication during pregnancy, which means it has shown to have some adverse effects on animal fetuses, but has not been adequately studied in humans. Ultimately, use of Schedule C medications are believed to be warranted if the benefits outweigh the risks of using the drug.
The FDA has approved the use of naloxone in infants who have been “narcotized” or who have received narcotics through their mother.
How can I get naloxone?
Naloxone is traditionally obtained by prescription, but in 2015 CVS announced stores in 14 states would be selling naloxone without a prescription. You can also check the GetNaloxoneNow.org website to find more info regarding naloxone availability based on whether you’re a first responder, loved one, substance user, community member or potential bystander.
Naloxone cost:
The cost of naloxone varies from free (with the help of programs such as Project Lazarus) to several hundred dollars. Most insurance plans will help cover some, if not all, of the cost, including private insurance and Medicaid.
Storing naloxone:
Naloxone should be stored at room temperature, away from direct sunlight and should not be exposed to extreme heat or cold. Do not store naloxone in the refrigerator.
Expired naloxone:
Naloxone has a shelf life of approximately 18-24 months and is required to have an expiration date at least 12 months out from the date of the prescription. Expired naloxone should be replaced with a new kit. According to the harmreduction.org website, using expired naloxone is better than nothing, if it is the only thing you have. Like many medications, its effectiveness decreases after the expiration date, but that does not necessarily mean it won’t work. It may be just effective enough to reverse the overdose and using an expired kit will be better than doing nothing at all.
Be sure to dispose of expired kits properly! Start by inquiring at your pharmacy for disposal options.
History of naloxone:
Naloxone was patented by inventor Jack Fishman in 1961 for the treatment of constipation due to opioid use. It was not known at the time that it would later save thousands of lives and become a hallmark drug in the response to the opioid epidemic. Naloxone became a household name in the 90’s, when distribution of the drug was opened to lay people.
Does naloxone encourage drug use?
The argument that access to naloxone increases or encourages drug use has yet to be proven. The thought is that naloxone instills a false sense of safety and encourages users to push past “safe” levels of use. Furthermore, some argue that providing an antidote sends the message that drug use is socially acceptable. As one scientific article points out, these arguments have no research to back them up, and to limit access to a life-saving drug based on unfounded theories is just plain unethical.
Do you or someone you know need help with an opiate addiction? Detox, followed by inpatient or outpatient treatment can provide a great foundation for recovery.



